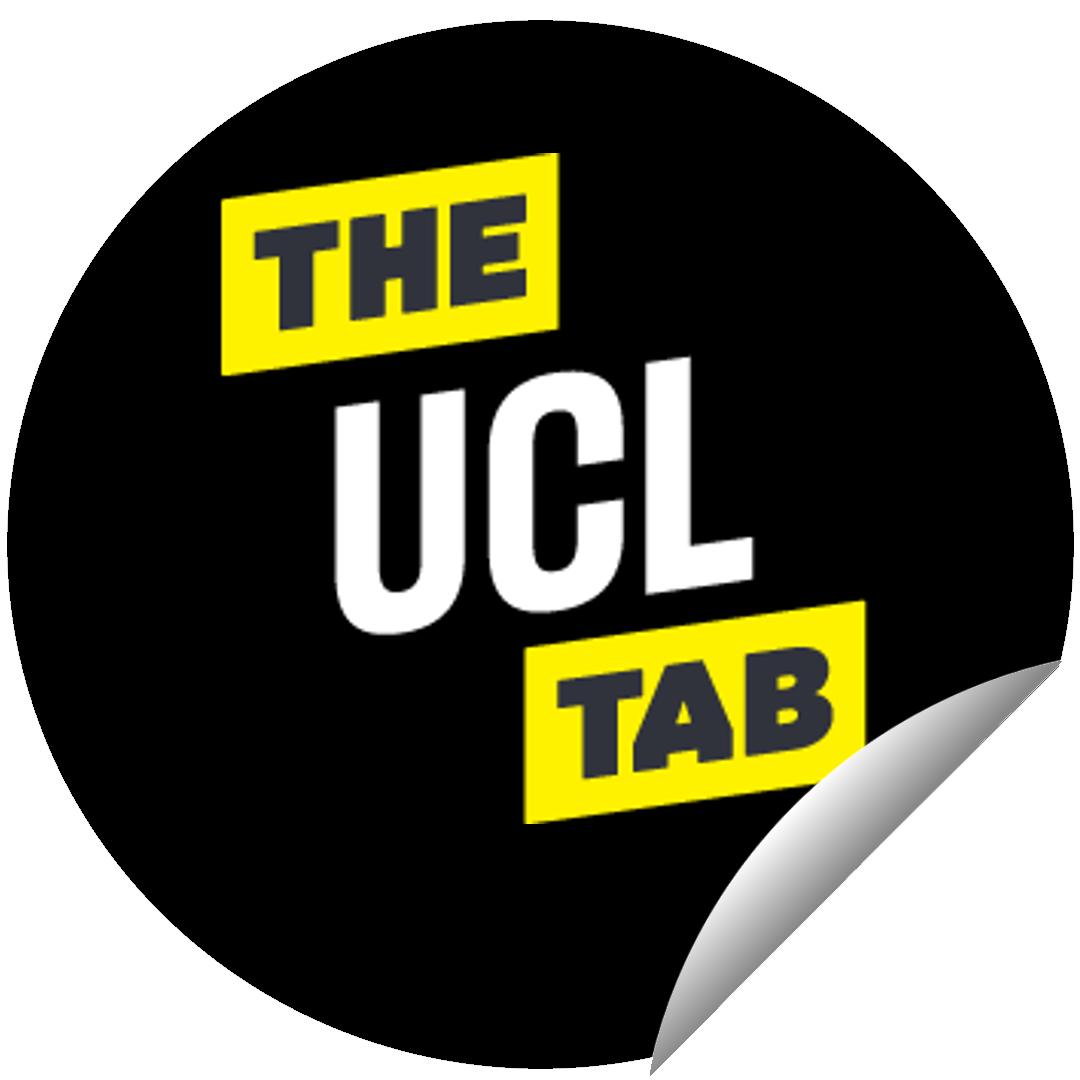
Goldsmith’s student with brain tumour dismissed as ‘fresher’ with ‘anxiety’ by GPs
Doctors told Lucy: ‘A girl like you wouldn’t have a brain tumour’
A student with a brain tumour was dismissed by GPs for over a year, and told her symptoms were due to “a mixture of anxiety and drinking too much.”
Lucy, 24, was also misdiagnosed with depression, panic attacks, and PCOS, before her pharmacist told her GP she needed to have a CT scan, which picked up her brain tumour.
Lucy said she initially assumed her GP knew better than her, but now says: “If there is something wrong you need to advocate for yourself.”
“You do know your own body,” She added.
Lucy’s symptoms started before she began her English degree at Goldsmith’s, in September 2018.
Her early symptoms included zoning out, frequent deja vu, and hallucinating the smell of bacon, despite being vegetarian.
When she went home to isolate from the pandemic in March 2020, her symptoms worsened to include seizures which caused her to pass out, and “migraines so bad the entire right side of my body would go numb,”
“I thought I’m either going into psychosis or I’ve got a tumour – it definitely wasn’t depression or anxiety,” Lucy said.
Lucy began to google her symptoms, and said everything pointed to epilepsy and a brain tumour (her eventual diagnosis), but a different GP dismissed her as “too young,”
“A girl like you wouldn’t have a brain tumour,” they said.

via SWNS
Research conducted by the University of Cambridge and King’s College London showed doctors in the UK ranked patients’ own assessment of their symptoms as the “least important” piece of evidence for diagnosis.
The same study found almost half of the patients studied reported never or rarely being asked for their own assessment of their disease.
The research’s lead author, Dr Melanie Sloan, said: “It’s incredibly important that we listen to and value patients’ insights and their own interpretations of their symptoms (…) they are the people that know what it is like to live with their condition.”
She added: “We also need to make sure that clinicians have the time to fully explore each patient’s symptoms, something that is challenging within the constraints of current health systems.”
Lucy was experiencing permanent visual hallucinations when she reached out to her local pharmacist for help.
Her hallucinations included seeing pink elephants, pins and needles in her face, and tasting metal.
Lucy says she cried down the phone to her local pharmacist, who spoke to her GP.
She said: “Once he’d spoken to my GP, they arranged for me to have CT scan.”
In June, the scan found a benign brain tumour, requiring a craniotomy to remove.
Lucy took a year out of her studies to recover, but was able to return in 2021, and graduated a year later.
She is now able to lead a normal life, but with epilepsy and short-term memory loss.
Lucy said: “I caught my brain tumour early (…) If I hadn’t there could have been a chance it wouldn’t have been removed and the ending would have been a different scenario.”
“People think a brain tumour is a death sentence – it’s not always that way.” she added.
Feature image via SWNS
Related stories recommended by this writer:
• The London Tab is looking for new writers: Come join us!
• LSE has been named the best university in the UK by The Times and Sunday Times
• ‘So unexpected’: Ed Sheeran serenades UCL grad from canal boat whilst she was running