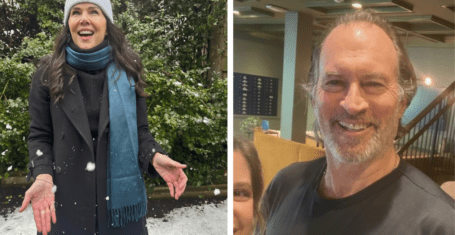
Interview: Dr Ben Warne, the man behind Cambridge’s asymptomatic testing scheme
He sends us emails, we send him our swabs, but what does Dr Ben Warne think of the programme, student participation, and its impact?
Unless you’re a medic, you probably only know Dr Ben Warne from his signature at the end of emails about the asymptomatic testing programme. Alongside Dr Nicholas Matheson, the scheme’s architect, Dr Warne is one of the key figures behind the scheme’s implementation and its day-to-day running, works as a junior doctor at Addenbrooke’s, researches for his PhD and somehow finds the time to email the student body.
With the news that mass testing is to be adopted by many universities at the end of term in a bid to get students home for Christmas, many will be looking to the Cambridge University programme and its logistics and implementation.
We spoke to Dr Warne about the development of the testing programme, how it runs, and what he and his team have learned so far.
Before the programme
When Covid-19 first reared its disruptive head, Dr Warne was halfway through his PhD, in hospital-acquired infections and how these – in particular influenza – spread in hospital settings. He tells us that ‘I was brought back from my PhD into the hospital, where I spent most of my time looking at the Covid patients and data’, and that before helping set up the university’s asymptomatic programme, he was “very peripherally involved in the healthcare worker screening” that was set up at Addenbrooke’s earlier in the pandemic.
It is with this background that Dr Warne became involved with Cambridge’s screening programmes, and he emphasises the importance of collaboration between the university and the hospital in their development.
“Back at the end of March we had very limited testing capacity, so there was a collaboration set up between the university and the hospital. Professor Stephen Baker’s research group repurposed its laboratory so it was no longer being used for academic work on bacteria but instead was testing for Covid-19 in NHS staff. As a result, we were one of the first hospitals in the country with healthcare worker screening.”
Beginning with the testing of symptomatic testing of healthcare staff, then their asymptomatic testing, and then symptomatic testing of university staff, Dr Warne and his team had the experience of setting up various screening programmes before beginning on that for students.
What the scheme does need, however, is space. Tests take place in the Anna Mclaren building on the Cambridge Biomedical Campus, which while part of the network of national coronavirus testing laboratories allows the testing scheme to use ‘a tiny fraction’ of their capacity, in a facility which has “blossomed into a unit that tests thousands and thousands of samples per day”.
Warne describes how the building “was initially very heavily supported by PhD students and graduate students and academics from the university, who helped run the lab in conjunction with AstraZeneca and GlaxoSmithKline”, and it is part of the agreement between the university and testing facility that means the team can use “a tiny fraction of their testing capacity for research and innovation into the way that we use testing”.

The logistics
Dr Warne describes how the asymptomatic screening programme works in four parts, beginning with the manufacturing of the test kits in-house. He tells us that Professor Duncan Macfarlane and his team from the university Institute for Manufacturing have “set up what is essentially a small factory in a matter of weeks, where we get the raw components in, make up the testing kits and work with the University Information Services to be able to print the barcodes on them and be able to allocate people to pools. They also help to work out the logistics of getting the testing kits to colleges and picking up the samples and taking them to the testing facility.
“There’s also a lot of work that goes on with the colleges, helping to support them and also in communicating with students, so that samples are in the right place and the right signage is available. The colleges have been incredible at helping get the programme up and running in such a short time. Each day that the testing happens, the samples get picked up, taken to the Anne McLaren building and the tests get immediately booked in.
“We try and get the samples there by 3pm, they’re tested in the evening and they’re processed overnight so that the results are available first thing in the morning. Those results then are taken to a secure server where they’re matched back up with student information and then results are sent back out to students via text message.”
“We were delighted when it became apparent that we were looking at 75 to 80 per cent participation”
When asked about whether he expected the high level of participation from the student body, Dr Warne said that “We honestly didn’t know how many students were going to participate, because we didn’t really have a precedent for this in a UK university, and we know that voluntary screening programmes in general have very variable participation rates.
“We were delighted when it became apparent that we were looking at 75 per cent to 80 per cent participation, because it showed a huge amount of interest in the programme, and also because when you start reaching those levels of participation you can really make a significant public health difference to the spread of the disease.”
Regarding those who have not consented to participate in the scheme, Dr Warne stresses that “we’re very respectful” of the variety of reasons why people may not want to participate. However, he notes that “There are very few people who actually actively declined to participate, and the majority of those remaining just haven’t got in touch with us.
“I would encourage anyone who hasn’t made a decision about it to really think about it, find us on the website, and it’s never too late. The programme works, it’s successful, and we know that as we approach Christmas in particular, there’s a great opportunity to limit the amount of Covid-19 in the university and therefore what we take home with us at Christmas to our families and loved ones.”

(Image credit: Camfess)
“National testing will always take priority”
There have been some concerns that the asymptomatic testing scheme at the University takes up resources that the rest of the country may need, and Dr Warne stresses that “The agreement that we have with the laboratory is that we are only able to do our testing if there is enough capacity in the national system to enable us to do so. We are only using a tiny fraction of their testing capacity – as part of the screening programme we are doing roughly 2000 tests per week in a network that’s set up to do tens or hundreds of thousands of tests a day.
“If the capacity is required for other areas of national testing that will always take priority. Fortunately we’ve been in a position since the start of the programme that hasn’t been needed, and actually the laboratory has been able to expand its own capacity to comfortably accommodate us.
“We completely understand that we need to be testing symptomatic people as quickly as we can, but one of the great strengths of this programme is that it should in theory reduce the amount of testing we have to do. By pooling tests we’re testing more people per sample, but also by providing more effective control within the university we’re able to reduce the number of Covid-19 infections and therefore the number of tests we need to do on people in the wider Cambridge community.”
“It’s really important to think about the broader community”
Also working at Addenbrooke’s looking after coronavirus patients, Dr Warne has seen first-hand the effect that the virus can have. When asked about the attitude amongst some younger people that COVID is not something to worry about, he remarks that whilst it “does disproportionately affect older individuals”, “we have seen young adults on our Intensive Care Unit because of Covid and Covid-related issues.”
While this is a “tiny minority”, he also mentions that the average age of someone admitted to the Addenbrooke’s ICU due to Covid is 61. As he says, “that’s not that old” and “it’s certainly well within the working age of staff at the university”, and therefore something that students should bear in mind.
“I would urge people to think about the people they come into contact with; in the university, the broader Cambridge community but also their friends and family when they go home at Christmas. The grandparents, the older relatives or the vulnerable relatives; those are the people that we are seeing coming into hospital, getting sick and are dying of Covid-19.
“I think that it’s really important to think about the broader community and the responsibility that we have to it regarding the decisions we make with this testing programme.”

“Harnessing expertise across the university”: The importance of collaboration
Dr Warne stressed throughout the importance of collaboration in both the setting up and the continued success of the programme. It was because of the “existing good ties” between the university and the hospital – both with neighbouring buildings and many shared staff – that the testing programme was set up so rapidly, because of the “existing links that we were able to build up, and I think it’s expanded from that initial programme of staff testing and for NHS workers in April and it’s all developed from there”. Although Cambridge isn’t unique in its testing programme – Dr Warne mentions those in America and other universities across the UK – what strengthens Cambridge’s is its close ties between the hospital and the university, and the subsequent support from the student body.
“The key thing has been the amount of support and goodwill being given to the programme by everybody. Lots of people in the university were very keen to support it, and that ultimately translated into lots of support from the students. Once we sent those emails out in September inviting people to participate we had a huge amount of interest and participation which has been absolutely fantastic.”
He stresses that “the reason why this programme exists is through a series of collaborations”, as it’s “an enormous achievement we’ve been able to do here and I think it’s through good will, hard effort and student involvement and I’m very very grateful to everybody who’s participating”.
Dr Warne ended the interview by saying that “Every day is a fresh set of challenges”, but that “What I’ve seen in the last eight months is a really inspiring attitude most of the time from most people, about pulling together both in the NHS and in the university to fight the virus together.
“That’s what keeps me going day to day and I get that every day- I meet new people who’ve got inspiring stories to tell. I know that it’s challenging, that it’s not always good news, and it’s not always positive stories, but a lot of positivity is coming out of it.”
And although he hasn’t said so himself, Dr Warne’s story is one of these inspiring ones.
If you’ve not yet filled out the consent form for the asymptomatic testing form, we’d encourage you to do so, even if it’s just to confirm that you don’t want to take part in the scheme. You can find the consent form here, and more information on the #StaySafeCambridgeUni campaign here.
All image credits: University of Cambridge, unless otherwise specified.